Navigating the compliance guidelines and regulations surrounding investigator meetings can be daunting for pharmaceutical companies.
As someone who has worked in this field, I empathize with pharmaceutical companies’ challenges in ensuring these events adhere to the myriad guidelines and regulations.
The History of Investigator Meetings
Investigator meetings are not just “nice-to-have” — they’re an absolute must for any pharmaceutical company looking to bring safe and effective medicines to market.
These meetings bring together principal investigators (PIs) — doctors and nurses — to review the critical details of clinical study protocols and ensure compliance with all relevant regulations.
Before the 1990s, pharmaceutical representatives tried to persuade doctors to promote their drugs through nice accommodations and enjoyable meals. This overspending perception raised concerns about conflicts of interest. Pharmaceutical leaders and opinion leaders came together in the 1990s to establish a Code of Ethics and Pharma Guidelines.
In 2010, the government stepped in with the Sunshine Act, which introduced new rules and regulations for pharmaceutical companies. The Sunshine Act mandates transparency by requiring pharmaceutical companies to disclose financial relationships with healthcare providers, ensuring accountability and integrity in the healthcare industry.
The Sunshine Act applies to any meeting or interaction between pharmaceutical companies and healthcare professionals, including but not limited to conferences, seminars, symposiums, advisory board meetings, dinner meetings, and any other event where payments or transfers of value occur.
The Challenges of Compliance
Complying with the Sunshine Act is no easy feat. Pharmaceutical companies must report every dollar they spend on healthcare professionals, including flights, hotels, and meals for investigator meeting attendees.
Most companies have per-person spending limits, which can make it nearly impossible to host a function at a hotel in a major city. For example, some companies have meal caps regarding food and beverages. A “breakfast” meal may be limited to $25 per person, which barely covers the cost of a continental breakfast at most hotels.
In the United States, the current all-inclusive tax and service charge for food and beverage is $125 per person per day, which, after taxes, amounts to a meager $80 for food. There are also caps on airfare and the type of hotel.
I empathize with pharmaceutical companies that have to navigate this red-tape nightmare. Keeping up with changing regulations and following good clinical practice takes time they don’t have, and when language barriers are added, overwhelm is the inevitable result.
Failing to comply with these regulations has severe consequences, including but not limited to:
- Fines
- Penalties
- Product recalls
- Damage to consumer trust
- Loss of reputation
- Decline in sales
- Negative impact on share values
- Loss of investor confidence
- Suspension
- Criminal charges
- License revocation
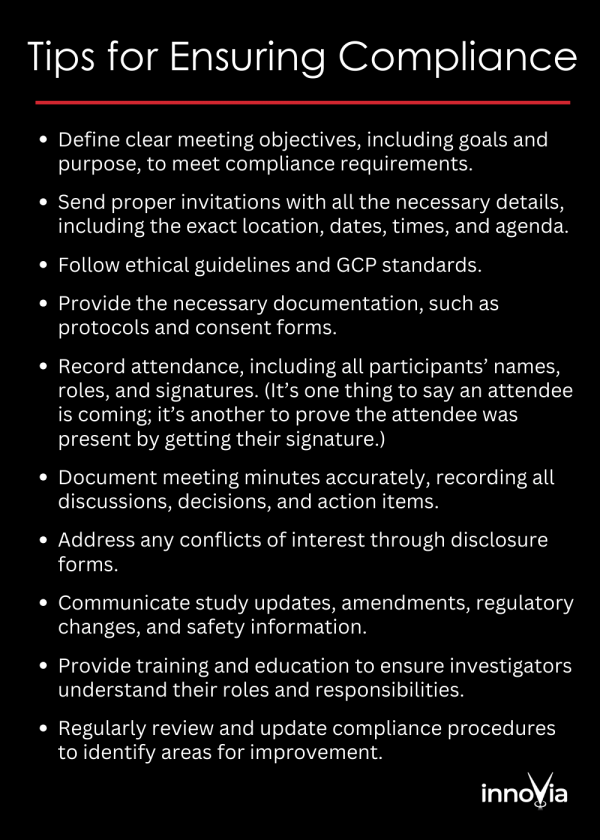
Tips for Ensuring Compliance
So, what can pharmaceutical companies do to ensure their investigator meetings comply with the latest regulations?
Here are some tips:
- Define clear meeting objectives, including goals and purpose, to meet compliance requirements.
- Send proper invitations with all the necessary details, including the exact location, dates, times, and agenda.
- Follow ethical guidelines and GCP standards.
- Provide the necessary documentation, such as protocols and consent forms.
- Record attendance, including all participants’ names, roles, and signatures. (It’s one thing to say an attendee is coming; it’s another to prove the attendee was present by getting their signature.)
- Document meeting minutes, recording discussions, decisions, and action items.
- Address any conflicts of interest through disclosure forms.
- Communicate study updates, amendments, regulatory changes, and safety information.
- Provide training and education to ensure investigators understand their roles and responsibilities.
- Regularly review and update compliance procedures to identify areas for improvement.
The Role of Production Partners
As a production company that works with pharmaceutical clients on investigator meetings, we face unique compliance challenges, especially regarding confidentiality and data protection.
Investigator meetings often discuss sensitive patient data, clinical trial protocols, and proprietary information, so protecting confidentiality and adhering to data protection regulations are crucial. We implement strict data handling and confidentiality protocols, ensure all meeting participants sign non-disclosure agreements (NDAs), and use secure technologies to safeguard data during meetings and when sharing materials.
Navigating last-minute changes to presentations can also be challenging, as the updated files may be on a secure system or server we don’t have access to. We plan for these scenarios in advance and have a secure process for receiving and handling this content.

Final Thoughts
Navigating compliance issues for investigator meetings can be overwhelming. However, hosting successful, compliant events is possible by staying informed about the latest regulations, implementing protocols, and partnering with an experienced production company that understands the pharmaceutical industry.
We at innoVia Production specialize in producing investigator meetings in the life science space. Our advice to pharmaceutical companies is to ask themselves: Why am I collecting the data? If you don’t collect it, you don’t have to protect it.
Also, be selective when choosing a production partner — or any vendor, for that matter. Choosing a vendor that understands the pharmaceutical industry’s compliance regulations eliminates risk. Putting in place a strategic management program, such as an MSA (master services agreement) or PVA (preferred vendor agreement), is beneficial, too.
By doing so, you can focus on what matters — bringing safe and effective medicines to the patients who need them.